With Lupus, You CAN Have Your Health!
Here’s The Scoop
There are two key concepts you should know:
There is a proportional relationship between food and inflammation. This means there is a direct
impact of what you eat on your inflammation.
There is also a proportional relationship between inflammation and pain. This means that your level
of inflammation can be directly related to your pain.
Therefore, it can be said that:
what you eat impacts your pain
And more importantly:
what you eat impacts your health
Arteries are Affected by Inflammation
Did you know that the walls of your arteries are greatly affected by inflammation? It may not be
cholesterol or plaque that leads to heart disease. Especially for lupus patients, inflammation is the
Number One cause of heart disease.
Why does this particularly matter? Dr. Mankad explains that it matters because we have an
inflammatory condition. We already have an underlying level of inflammation by virtue of having lupus.
Add on top of that the use of steroids, which brings its own risk of cardiovascular disease, and you’ve
got a concern.
Fact: people with systemic lupus are 9-50 times MORE AT RISK than the general population of having a
myocardial infarction. And, they have a high cardiovascular mortality. Lupus is now considered to be an
independent risk factor for the development of atherosclerosis. Viewing atherosclerosis as an
inflammatory disease, this association becomes stronger and better understood.
See: Cardiovascular Disease in Systemic Lupus Erythematosus: The Role of Traditional and Lupus Related Risk Factors:
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2779351/ (second paragraph of the Introduction).
Here is another reference saying that inflammation is linked to atherosclerosis (hardening of the
arteries), a cause of heart disease and stroke. And that fat tissues also increase insulin resistance,
leading to type 2 diabetes. See: “The G.I Diet” by Gallop (p. 135).
So, we need to take extra care in controlling our inflammation. Plus, we’ll feel better if we do.
OK. SO HOW DO WE DO THAT?
CONTROL YOUR BLOOD SUGAR.
Why?
Decrease Pain and Increase Energy
What Happens When We Do That?
Deeper Background
HOW DO WE KEEP OUR BLOOD SUGAR UNDER CONTROL? HOW DO WE CREATE AN ANTIINFLAMMATORY DIET?
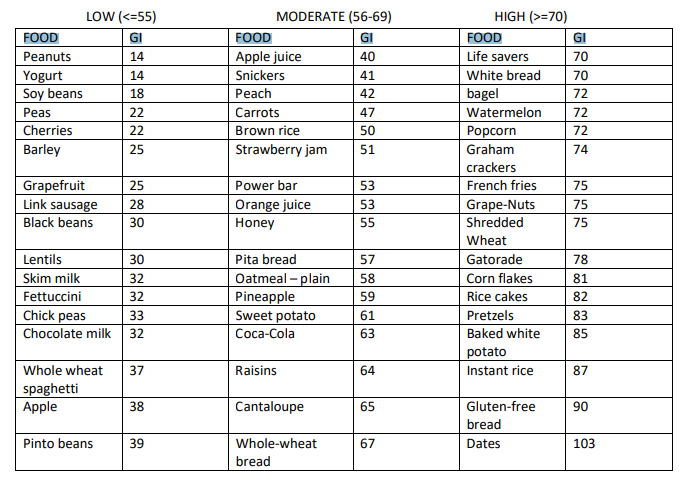
YOU’RE GOING TO GET VERY FAMILIAR WITH THE GLYCEMIC INDEX CHART
You’ll get so familiar with this you’ll learn by heart glycemic index (GI) value of every food you eat.
Remember, the pay-off is huge.
FOR HOW LONG? It is recommended that you eat low to medium GI foods for 30 days.
THIS WILL GET YOU FEELING BETTER, AND WILL CHANGE YOUR LIFE.
COMMIT!
Example of a Glycemic Index Chart
| Food | GI | Food | GI | Food | GI |
|---|---|---|---|---|---|
| Peanuts | 14 | Apple Juice | 40 | Life Savers | 70 |
| Yogurt | 14 | Snickers | 41 | Bagel | 70 |
| Soy Beans | 18 | Peach | 42 | White Bread | 72 |
| Peas | 22 | Carrots | 47 | Watermelon | 72 |
| Cherries | 22 | Brown Rice | 50 | Popcorn | 72 |
| Barley | 25 | Strawberry Jam | 51 | Graham Crackers | 74 |
| Grapefruit | 25 | Power Bar | 53 | French Fries | 75 |
| Link Sausage | 28 | Orange Juice | 53 | Grape-Nuts | 75 |
| Black Beans | 30 | Honey | 55 | Shredded Wheat | 75 |
| Lentils | 30 | Pita Bread | 57 | Gatorade | 78 |
| Skim Milk | 32 | Oatmeal – Plain | 58 | Corn Flakes | 81 |
| Fettuccini | 32 | Pineapple | 59 | Rice Cakes | 82 |
| Chick Peas | 33 | Sweet Potato | 61 | Pretzels | 83 |
| Chocolate Milk | 32 | Coca-Cola | 63 | Baked White Potato | 85 |
| Whole Wheat Spaghetti | 37 | Raisins | 64 | Instant Rice | 87 |
| Apple | 38 | Cantaloupe | 65 | Gluten-Free Bread | 90 |
| Pinto Beans | 39 | Whole Wheat Bread | 67 | Dates | 103 |
Contact me for more information, and for diet and exercise consultations personalized for you:
[email protected]
720 470 8049
Real-Life Easy
NOW, WE DON’T WANT TO LEAVE YOU HANGING, GIVING YOU A FEW NUMBERS ON A CHART AND
SOME DIRECTIONS. WE WANT TO MAKE THIS REAL-LIFE-EASY FOR YOU. SO HERE ARE SOME HEALTHY
ALTERNATIVES THAT YOU SHOULD PICK UP IN YOUR GROCERY STORE AND TRY:
Eat This, Not That
WE DON’T BELIEVE IN ELIMINATING FOOD, WE BELIEVE IN REPLACING IT:
-If you can’t live without white, or even wheat bread (even whole grain bread can be high on the
glycemic index chart), eat rye bread and rye crackers. Delish!
-If you love rice: replace it with Quinoa and Barley. At the very least, replace white rice with brown.
-If you love pasta: replace it with Brown rice pasta.
-If you’ll go crazy without white sugar: use agave! Agave is not necessarily “low” on the glycemic index
chart, so use it with care, but it is lower than sugar.
Artificial sweeteners come with their own set of problems, and agave is a great alternative, so we don’t
see a need for the fake stuff.
-If you’d go nutty without peanut butter: eat it anyway – just don’t buy roasted – and make sure it is
“natural”, made with raw almonds. Almond butter is a delicious alternative.
-Use turkey to replace red meat. The fats within red meat can increase blood cholesterol. Buffalo meat
is also a wonderful alternative to red meat. And of course there’s fish. SUPER GOOD for reducing
inflammation and giving us a healthy dose of those Omega-3s!
-If you have to have oil – the healthy oils are beneficial and can help reduce inflammation – Olive,
sunflower, and grape seed.
-If you must have butter – reduce it by a third, or eliminate it, and see above point!
-If you need your carbs: lentils, a starchy food, are filling, and can give us that carb “fix”.
-If you like your potatoes: Sweet potatoes are lower on the glycemic index chart than are white
potatoes. As are yams. And don’t forget root vegetables – turnips can be a wonderful source of
vitamins and fiber!
-If you need some spice: blueberries and cinnamon add a wonderful aspect to your morning bowl of
oatmeal.
We recommend eating oatmeal over typical breakfast cereals. Oatmeal can help reduce cholesterol and
is a low-GI food! Buy steel-cut if you like, which is even lower on the glycemic index chart than quickoatmeal. And avoid those sugary cereal starch traps.
Eggs: gotta have it. They are a wonderful source of protein, and since food cholesterol does not
contribute to blood cholesterol, an egg a day keeps the doctor away!
We also have read that eating protein with every meal helps absorb the food you eat, and helps
maintain blood sugar levels throughout the day.
We’ve all heard it: eat 5 to 6 small meals a day to continually maintain blood sugar levels.
EASY!
AND OF COURSE, RUN THIS AND ALL DIET AND EXERCISE PROGRAMS YOU PERFORM BY YOUR DOCTOR.
HERE’S THE GOOD NEWS:
Reducing the sugar in your diet will also make a huge difference in increasing your energy, the second
piece of a “Health with Lupus” lifestyle:
Having more energy and less pain will allow you to exercise.
It’s hard to exercise when you’re in pain. So we do it in a smart way. It’s worth it: long-term effects of
moderate exercise are shown to create a reduction in inflammation.
SMART Method:
THERE IS MORE TO IT THAN THIS – BUT, TO GET YOU STARTED, THE BASIC GIST IS TO REDUCE PRESSURE
POINTS ON YOUR JOINTS BY KEEPING THE WEIGHTS OVER OR NEAR THE JOINT THAT HURTS.
You’ve all held a water bottle at arm’s length, right? Feel how it reduces the “force” on your joint when
you bend your arm, bringing the water bottle close to your body?
This is the way to perform exercise. And remember, “weights” can include body weight to start. Then
move up in terms of what you can tolerate. Try starting with small tuna cans (five ounces), then
graduate up to 2-pound weights. That’s all you need!
This will help you prevent injury and create a sustainable program you can do for life.
Call us, we can help.
Other wonderful things will happen once your pain goes down. Stress and anxiety will decrease too, and
sleep and ability to tackle the world will skyrocket.
You deserve to take care of yourself.
This journey is about you. Bring out your personal power.
Summary
eating right (and exercising in a manner appropriate specifically for you) can help reduce
inflammation. It can empower you with skills to protect your body from the overproduction of autoreactive, or “auto”, antibodies. Reducing the number of auto-antibodies can result in decreased
inflammation, which can directly decrease pain that is often associated with inflammation.
In fact, following these dietary recommendations is a good idea for everyone, including those without
chronic conditions. These methods have been shown to increase energy and decrease pain as shown in
the references provided. Following these methods can also contribute to weight loss, optimizing your
exercise routine.
Additional References
Examination of the relationship between sugar and inflammation: Consumption of refined carbohydrate
by patients with Crohn’s disease in Tel-Aviv-Yafo:
https://www.ncbi.nlm.nih.gov/pubmed/7267494?dopt=Abstract
Exploration of the relationship between foods and reduction of inflammation and pain: 17 ScienceBased Benefits of Omega-3 Fatty Acids: https://www.healthline.com/nutrition/17-health-benefits-ofomega-3
Chronic inflammatory nature of lupus and the relationship between inflammation and pain: How lupus
affects the muscles, tendons and joints: https://resources.lupus.org/entry/joints-muscle-pain-in-lupus
As inflammation within the body decreases, the symptoms that can be associated with inflammation,
including pain, can also decrease. A must-read is the link between inflammation, pain, and chronic
disease: see: Inflammation, pain, and chronic disease: an integrative approach to treatment and
prevention: https://www.ncbi.nlm.nih.gov/pubmed/16320856.
